

The study was approved by the local internal review board. The objectives of the current study are to assess the anatomical and functional outcomes of patients with large, refractory macular holes that have been treated with full-thickness ART, as well as to describe the structural change of macular anatomy by optical coherence tomography after 1 year of follow-up. They claim that a full-thickness retinal graft may provide a sturdier scaffold for retinal gliosis with better tissue integration and possible ectopic synaptogenesis, which may lead to better anatomical and functional outcomes .
However, due to its initial success, several authors are now proposing this technique for idiopathic large MH as well . The autologous full-thickness retinal transplant (ART) is a novel surgical technique proposed by Grewal and Mahmoud that aims to treat patients when other surgical options are not feasible or are known to have a poorer prognosis . Such improvements have encouraged retinal surgeons to try expanding surgical indications to MH with clinical characteristics associated with poorer prognosis (MH associated with high myopia, or retinal detachment, inflammatory diseases, and extremely large macular holes . Through the last decade, the surgical prognosis of an idiopathic macular hole (MH) has improved significantly, mainly because of the constant refinement of surgical techniques as well as the development of new and specialized surgical instruments and dyes . More studies are needed in order to assess functional changes through time.
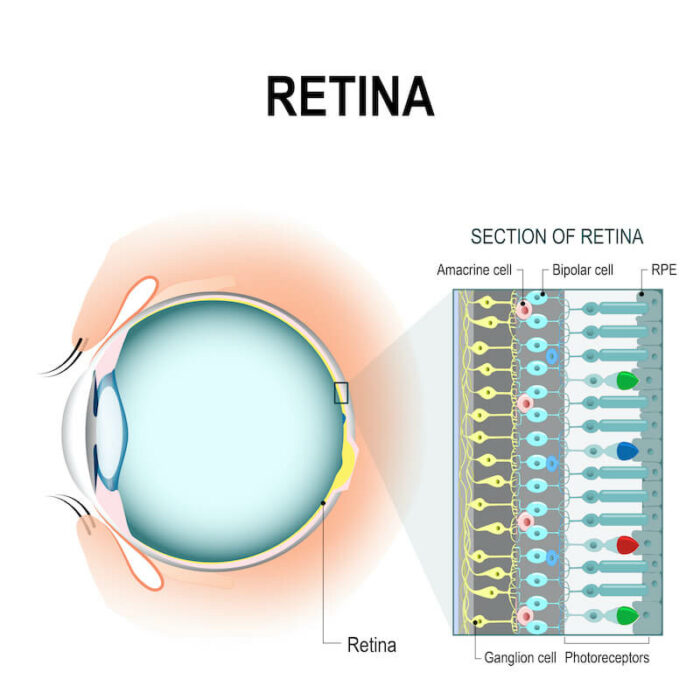
#Retina transplants full#
The full safety profile of this new technique is still unknown. ConclusionsĪn autologous full-thickness retinal transplant may improve the anatomical and structural outcome of patients with refractory macular holes. During follow-up, one patient developed mild proliferative vitreoretinopathy and epiretinal membrane without anatomical or functional consequences. Despite a positive trend toward visual recovery ( p = 0.034), after the correction of the alpha value, the change lost its statistical significance. Most patients formed a pseudofovea and normalization of the internal retinal layers. The remaining showed a 44.9% reduction of the initial gap. Six patients with a closed macular hole at the end of the follow-up had complete recovery of the myoid/ellipsoid layer. The closure rate after 12 months of follow-up was 76.92%. We enrolled 13 eyes from 13 patients (mean age: 67.15 years) with refractory macular holes, with a mean base diameter of 1615.38 ± 689.19 µm and a minimum diameter of 964.08 ± 709.77 µm.

Statistical analysis was done with a test for repeated measurements and Bonferroni correction, with an alpha value of 0.05 for statistical significance and a Mann-Whitney U test for nonparametric continuous variables. Follow-up was done at 1, 3, 6, and 12 months. All the patients underwent a 23-gauge pars plana vitrectomy with a full-thickness retinal transplant and silicone oil tamponade (5000 cs<). All the patients had a comprehensive ophthalmological examination, which included a best-corrected visual acuity assessment, fundus examination, and optical coherence analysis. We include patients with a clinical diagnosis of refractory macular holes with a minimum diameter of at least 500 µm. The objective of the present study is to assess the anatomical and functional outcomes, as well as the structural change through time, of the optical coherence tomography of patients with refractory macular holes treated with a full-thickness autologous retinal transplant. Despite the constant refinement of techniques and surgical aids, extremely large and refractory macular holes continue to have poor surgical outcomes with the current standard of care.


 0 kommentar(er)
0 kommentar(er)
